Abstract
Background: Out-of-hospital cardiac arrest (OHCA) is a significant global public health issue, few studies describe characteristics and trends in China. This study examines OHCA features and trends in Shenzhen, one of the fastest-growing cities.
Methods: This retrospective study analysed data from the Shenzhen Emergency Center database (2011-2018), including ambulance dispatch and pre-hospital medical records. Descriptive statistics and temporal trends were used to examine the incidence, patients characteristics, pre-hospital treatment, and outcome.
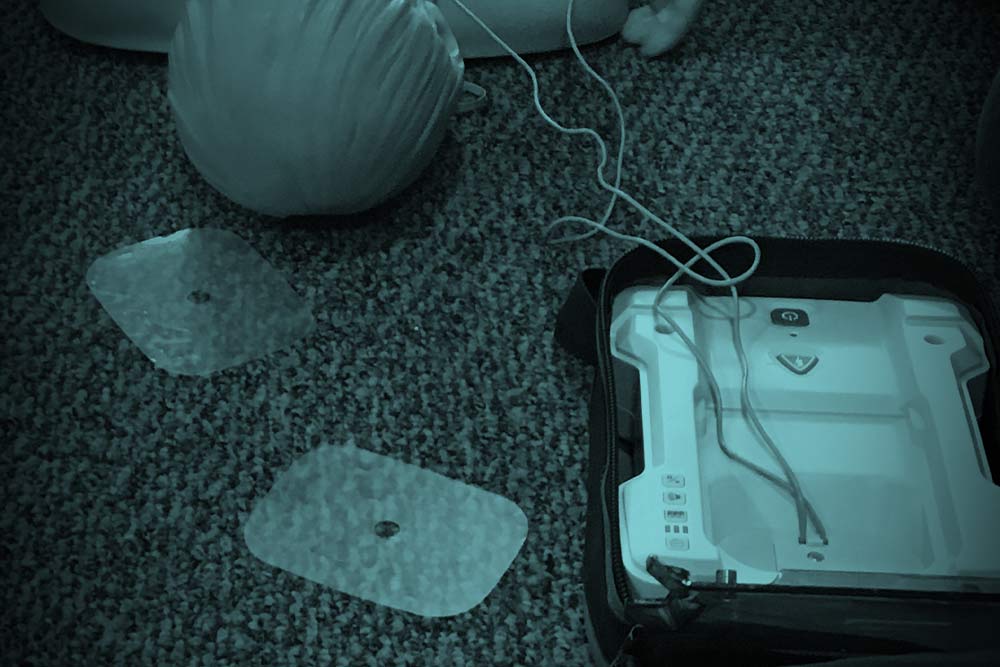
Results: Among 18,772 medical cause OHCA cases, the crude incidence rate was 17.4 per 100,000 population, with an age-standardised rate of 38.4. Incidence increased over time. Resuscitation was attempted in 43.8% of cases, with a median patient age of 56 years and 73.5% being male. Most arrest (69.0%) occurred at home, and 82% were presumed to be cardiac cause.The median response time was 11.2 min. Bystander cardiopulmonary resuscitation (CPR) rates increased from 4.6% in 2011 to 14.5% in 2018, while bystander automated external defibrillator (AED) use remained low (0.2%). Pre-hospital electrocardiogram (ECG) recording improved from 40.6% to 91.9%, with shockable rhythms 2.2%. Intravenous access was established in 69.7% of patients, 51.9% received epinephrine, 19.29% received pre-hospital defibrillation, and 16.4% underwent advanced airway management. The pre-hospital Return of Spontaneous Circulation (ROSC) rate increased from 2.7% to 5.8%, with a total ROSC rate of 3.11%.
Conclusions: OHCA incidence in Shenzhen is lower than both domestic and international levels but increasing. Low bystander intervention rated and prolonged response times contribute to poor outcome, underscoring the need for system improvements.
Full article;